Medicare Simplified 2025: Your Essential Guide to Common Questions
HALTHCARE
If you’re nearing retirement age (or helping a parent who is), you’ve probably Googled a few Medicare questions. Don’t worry – you’re not alone! Millions of Americans have the same questions, and we’re here to answer the most-searched ones in plain English.
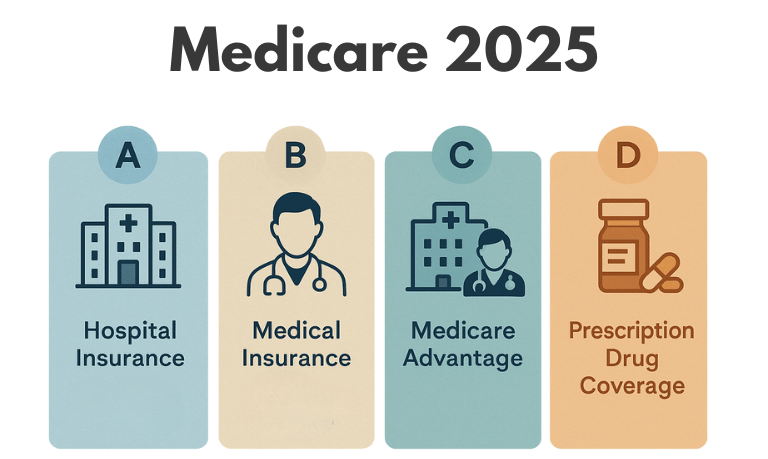
What are the parts of Medicare (Parts A, B, C, and D)?
Medicare is split into “parts,” and each part covers different things.
Part A – Hospital Insurance: Helps cover inpatient care in hospitals, skilled nursing facility care, hospice care, and some home health care. Part A is usually premium-free for most people who paid Medicare taxes while working (generally if you or your spouse worked ~10 years). If you didn’t work enough quarters, you can still get Part A by paying a monthly premium
Part B – Medical Insurance: Helps cover doctors’ services and outpatient care, like doctor visits, tests, preventive services (e.g. screenings, flu shots, yearly wellness check-ups), durable medical equipment (wheelchairs, walkers, etc.), and more. Part B has a monthly premium for everyone. In 2025, the standard Part B premium is $185 per month.
Part C – Medicare Advantage: This isn’t a separate benefit, but rather an alternative way to get your Medicare. A Medicare Advantage Plan is offered by private insurance companies approved by Medicare (think of Part C as a package deal). These plans bundle your Part A and Part B (and usually Part D drug coverage) into one plan. Medicare Advantage plans often include extra benefits like dental, vision, or hearing coverage that Original Medicare doesn’t cover. The trade-off? You typically must use the plan’s network of doctors and hospitals (no picking any doctor in the country, as you can with Original Medicare).
Many Advantage plans have low or $0 additional premiums, but you still pay your Part B premium, and they set their own copays and out-of-pocket costs. In short: Part C plans can offer more perks and an annual limit on your out-of-pocket costs, but they come with network rules and prior approval requirements for some services.
Part D – Prescription Drug Coverage: Helps cover the cost of prescription medications. These plans are offered by private companies following Medicare’s rules. You can get Part D by joining a stand-alone drug plan (if you have Original Medicare) or by enrolling in a Medicare Advantage plan that includes drug coverage. Part D plans have a monthly premium (averaging around $30-$40, though it varies).
The good news in 2025: Medicare has capped out-of-pocket drug costs at $2,000 for the year. Once your medication costs hit $2,000, you won’t pay more for prescriptions that year.
Feeling like an expert on the parts yet? Don’t worry if it’s still a blur – just remember
A = hospital B = medical C = private combo plan D = drugs
Original Medicare vs. Medicare Advantage: Which is better?
One of the top questions is whether Medicare Advantage plans are “good” – or, put another way, how they compare to Original Medicare. The truth is, it depends on your preferences and needs. Here’s a quick comparison:
Doctor & Hospital Choice: Original Medicare lets you go to any doctor or hospital nationwide that accepts Medicare – no networks, no referrals needed for specialists in most cases. Medicare Advantage (Part C) typically has a network – in many plans you must use doctors and hospitals in that network (usually within your local area) for non-emergency care. If you go out-of-network, you might not be covered or may pay more, except in emergencies.
Costs & Extra Benefits: Original Medicare has a standard cost-sharing: you pay a monthly Part B premium and generally 20% coinsurance for outpatient services after meeting the Part B deductible. Importantly, Original Medicare has no out-of-pocket maximum – meaning there’s no cap on your 20% share in a bad year, unless you have additional coverage like a Medigap supplement or Medicaid. Medicare Advantage plans, on the other hand, set an annual limit on what you pay out-of-pocket for Part A and B services (for 2025, Medicare requires that cap be no more than $8,300 in-network for most plans, though many plans have lower caps). Once you hit that cap, the plan pays 100% for the rest of the year.
Supplemental Coverage: With Original Medicare, you have the option to buy a Medigap (Medicare Supplement) plan to help cover that 20% coinsurance and other cost gaps. You can also get standalone Part D drug coverage. You cannot use a Medigap supplement with a Medicare Advantage plan – Advantage plans are meant to cover many of the same gaps themselves.
So, are Medicare Advantage plans good?
If you value having a cap on out-of-pocket costs and extra benefits (and don’t mind staying in a provider network), an Advantage plan could be great for you. On the other hand, if you spend part of the year traveling or living in different states, or you have a list of doctors you absolutely want to keep no matter what, Original Medicare with a Medigap allow you to choose providers nationwide.
And remember, you can re-evaluate and switch coverage during Medicare’s open enrollment each year if your needs change.
(Hint: Page 11 of the official handbook has a handy at-a-glance chart comparing Original Medicare and Advantage Plans.)
When can I get Medicare? (Can I get it at 62?)
Many people ask if they can get Medicare early, for example at age 62. The short answer: Medicare kicks in at 65, when most people become eligible for Medicare. You cannot get Medicare at 62 just by virtue of age – 62 is the eligibility age for Social Security retirement benefits (early retirement), but it doesn’t grant you Medicare.
However, there are important exceptions for younger people: if you’ve been receiving Social Security Disability benefits for 24 months, you’ll be automatically enrolled in Medicare in your 25th month of disability – so that could happen at whatever age, even in your 30s or 50s, depending on when the disability started. Additionally, if you have ALS (Amyotrophic Lateral Sclerosis), Medicare starts as soon as your disability benefits start (no 24-month wait). And if you have End-Stage Renal Disease, you can qualify for Medicare at any age.
For most folks though, think 65. You actually have a 7-month Initial Enrollment Period (IEP) to sign up for Medicare – it starts 3 months before the month you turn 65, includes your birthday month, and ends 3 months after.
What if you miss the sign-up window? If you don’t qualify for automatic enrollment and you skip signing up at 65, you could face late enrollment penalties later on – so it’s usually best to enroll during that initial window unless you have a good reason (like employer coverage) to postpone. Always double-check the rules if you plan to delay Part B to avoid penalties down the road.
And remember, Medicare isn’t mandatory – but since most people get Part A free, almost everyone takes Part A at 65. Part B is optional, but if you don’t take it and you have no other health coverage, you’ll be responsible for all your doctor bills, which is risky.
How much does Medicare cost?
We all wish Medicare was free, but there are costs involved – premiums, deductibles, and copays.
Part A Premium: For most people, $0. Part A is premium-free if you (or your spouse) paid Medicare taxes for roughly 10 years (40 quarters) during your working life. If you have to buy Part A (few people do), it can cost a few hundred dollars a month (around $278–$518 in 2025, depending on how many quarters you have).
Part B Premium: The standard Part B premium in 2025 is $185 per month. Most people will pay this amount. If your income is above $106,000 (single) or $212,000 (married), you’ll pay an extra surcharge (IRMAA) on top of $185 – the surcharge scales up at higher incomes. Part B also has a yearly deductible ($226 in 2024 and in 2025) and typically you pay 20% of covered services (coinsurance) after the deductible – unless you have other coverage like Medigap or Medicaid to cover that portion.
Part D Premium: If you get a Part D drug plan, you’ll pay whatever that plan’s monthly premium is (it varies by plan, averaging ~$30). Like Part B, high-income folks pay an extra amount on Part D premium too (IRMAA for Part D). There’s also usually an annual deductible (max $505 in 2023; around that for 2025) for drugs and copays for each prescription. However – important new info for 2025 – your out-of-pocket spending on Part D drugs will be capped at $2,000 for the year, thanks to recent legislation.
Other costs: If you choose a Medicare Advantage plan (Part C), it will have its own cost structure. Many Advantage plans have a $0 premium (beyond your Part B premium), but some charge an extra monthly amount. They often have copays (e.g. $20 for a doctor visit, $300 per day for hospital stays, etc.) instead of the 20% coinsurance pattern. Each plan is different, but they must cap your annual out-of-pocket for Part A and B services (again, no more than $8,300 in-network in 2025, often lower). Medigap can cover most of your Medicare A and B deductibles and coinsurance, so it trades a fixed monthly cost for potentially big variable bills – many like that predictability.
Also note: Medicare Part A (hospital) has its own deductibles and copays if you have a long hospital or skilled nursing stay, and Part B has that 20% coinsurance. There’s no cap on that 20% with Original Medicare alone. That’s why about 8 in 10 people carry some additional coverage (Medigap, Medicaid, or an employer/retiree plan) to help with Medicare’s cost-sharing. If you have a limited income, you might qualify for programs that pay your premiums and coinsurance – which leads to the next question... Please check the next post
